Full steam ahead in Singapore’s Appropriate and Value-Based Care journey
)
Insights from the Appropriate and Value-Based Care Conference 2025, organised by Singapore’s Ministry of Health
Singapore has reached a ‘pivotal juncture’ in its healthcare journey. Backed by strong alignment amongst key stakeholders, including policymakers and public healthcare institutions (PHIs), and momentum for change through national initiatives such as the Three Beyonds and capitation funding, it is well-poised to harness the potential of a unified, national value-based care movement.
The Ministry of Health (MOH) has articulated its vision for Appropriate and Value-Based Care (AVBC) — not as a new initiative or replacement for Value-Based Healthcare, but as a unifying aspiration that brings together diverse programmes under a shared vision.
Top MOH leaders took the stage at the inaugural AVBC Conference, held on 16-17 October 2025 at Sands Expo and Convention Centre, outlining Singapore’s progress in AVBC thus far and future plans to further embed AVBC in everyday clinical practice. They were joined by local and international speakers from renowned healthcare organisations, and over 1,000 attendees across the healthcare value chain.
|
In her welcome speech, Ms Lai Wei Lin, Permanent Secretary (Policy & Development), MOH, underscored the pressing challenges facing Singapore’s healthcare system: an ageing population, a rising burden of chronic diseases, escalating healthcare costs, and rising patient expectations. Against this backdrop, AVBC is critical for ensuring sustainability and resilience of the healthcare system, while keeping patient-centred outcomes firmly at the centre of care. |
 |
|
Professor Kenneth Mak, Director-General of Health, highlighted the sharp rise in treatment costs and its pressure on healthcare system financing. The cost of heart valve replacements in Singapore had risen from $5,000 to $40,000 between 2013 and 2022, while lymphoma treatments saw a staggering 100-fold increase from $5,000 to $500,000. Meanwhile, unnecessary specialist outpatient visits, admissions, prolonged length of stay, and hospital-acquired adverse events add up to around $277 million in avoidable excess spending in 2022 alone. |
 |
 |
AVBC aims to reduce such excess spending while enhancing patient outcomes. By focusing on optimising both clinical results and resource utilisation, AVBC promises significant benefits for patients, healthcare institutions, and the broader system, as captured in the five core AVBC principles illustrated in the diagram on the left. |
Defining Value in Healthcare: A Global Perspective
A key theme of the conference was aligning on the definition of value in healthcare. Keynote speaker Associate Professor Scott Wallace of Dell Medical School, University of Texas at Austin, USA, emphasised that reducing costs alone does not equate value; the true measure of value lies in outcomes.
“High-value care leads to better outcomes, which reduces the need for more care and take costs out of the system,” he said.
“The goal is to measure success based on health results rather than only on resources used. We want to enable more health success without requiring higher overall spending.”
He further raised the need to focus on outcomes that matter to patients. From his research, these outcomes can be categorised into three ‘C’s:
- Capability: Ability to do what is important, often expressed as a functional outcome.
- Comfort: Reduction in physical and emotional suffering, tracked through reductions in pain and distress metrics.
- Calm: Ability to live life while getting care, in part the measure of a good patient experience.
Dr Stefan Larsson, Cofounder and Board Chair, International Consortium for Health Outcomes Measurement (ICHOM), elaborated on the need for standardised outcome measures. ICHOM has published 46 sets of standard Patient-Centred Outcome Measures specific to various medical conditions or specific subpopulations e.g. multimorbid elderly. Used by some 500 organisations in over 60 countries today, these are developed by international experts and clinicians in collaboration with patients, ensuring patients’ voices are reflected in the care they receive.
Advancing Singapore’s AVBC journey
Turning the focus back on Singapore, Mr Vincent Wu, Deputy Secretary (Policy), MOH, outlined the stark financial reality driving AVBC adoption, with healthcare spending having doubled repeatedly over the past decade and continuing to soar. Rather than simply raising taxes or cutting spending elsewhere, he emphasised choosing value through AVBC as a “third way” forward.
Mr Wu detailed the Ministry’s three-pronged strategy spanning population, system, and institutional levels. At the population level, initiatives like Healthier SG are shifting care upstream to primary care and community settings, supported by AI tools for early detection and telemedicine. At the system level, health technology assessment now informs resourcing decisions through programmes like the Cancer Drug List, which has achieved broad coverage of locally registered cancer treatments with significant price reductions.
Dr Daphne Khoo, Senior Advisor, ACE, then reflected on Singapore’s decade-long value journey.


| Both speakers highlighted that achieving a culture of AVBC across the healthcare ecosystem requires a concerted and sustained effort involving MOH, healthcare institutions, and professionals. To this end, the Ministry has identified several key elements of change critical to success, known as the ‘FOCUS-C’ framework: | 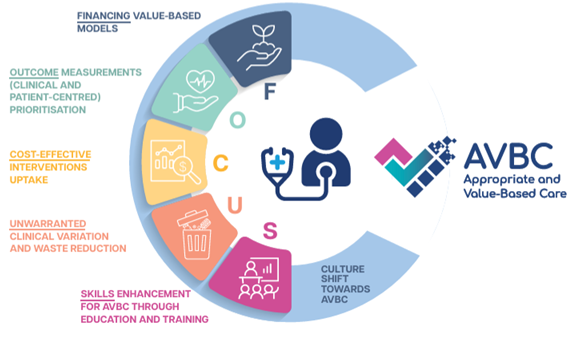 |
Singapore’s three AVBC champions—Adjunct Associate Professor Diarmuid Murphy, Professor John Abisheganaden, and Associate Professor Hairil Rizal Abdullah—shared how their clusters are already making significant strides on these elements.
For example, institutions under the National University Health System have driven over 80 AVBC projects, from primary to quaternary care. Its Appropriate Care framework tackles unwarranted clinical variation and waste on five fronts – laboratory tests, bedside testing, medications, care consolidation, and end-of-life care.
NHG Health has developed a systematic approach to the collection of patient-reported outcome measures (PROMs). After patients fill up questionnaires in the NHG Health app, the data automatically flows to the Next Generation Electronic Medical Records (NGEMR) system, a single unified platform developed to consolidate patient records across Singapore’s public healthcare institutions, allowing easy access by clinicians across the different cluster institutions and enhancing point of care conversations and analysis.
Meanwhile, SingHealth’s AVBC efforts in 2024 have saved 9,907 inpatient bed days, translating to $19 million in cost avoidance/savings. They also reported more cases avoiding complications (90) or deaths (102), and an increase in cases discharged within length of stay target (662).

The clusters pledged to continue efforts in exploring new innovations and models of care and driving cross-cluster collaboration and learning.
The Appropriate and Value-Based Care Conference 2025 was held on 16 and 17 October 2025 at Sands Expo & Convention Centre. For more information on the event, click here: https://avbc-conference2025.com/home

