Samsung Medical Centre’s path to smart healthcare
)
Dr Jong-Soo Choi, Chief Technical Officer at Samsung Medical Centre, shares his insights into smart hospital development
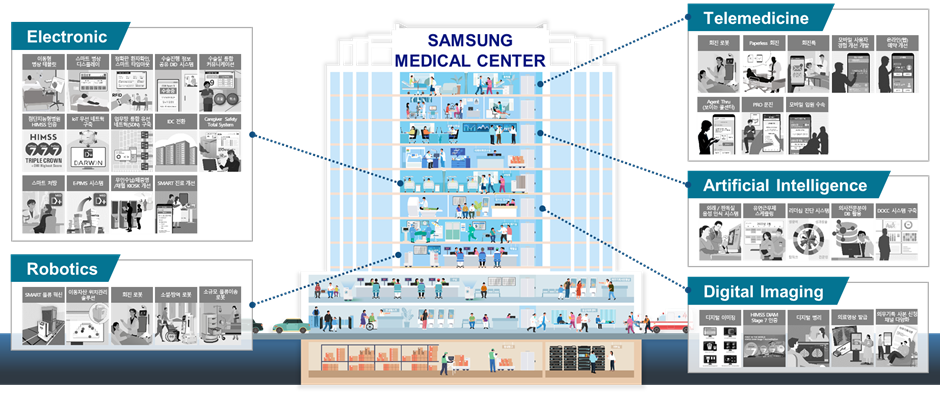
South Korea’s Samsung Medical Centre (SMC) is leading the global smart hospital revolution. In January 2024, it received the highest Stage 7 validation for HIMSS Adoption Model for Analytics Maturity, becoming the first healthcare provider in Asia-Pacific to do so. This achievement also makes it the only hospital in the world to achieve HIMSS Quadruple Stage 7, with its existing stage 7 validations in Infrastructure Adoption Model, Electronic Medical Record Adoption Model and Digital Imaging Adoption Model, each measuring different aspects of a hospital’s digital maturity.
|
Dr Jong-Soo Choi
|
With its strong commitment to digital transformation and technologies, the hospital was recently ranked 25th on Newsweek’s list of Best Smart Hospitals 2024. To find out more about SMC’s smart hospital strategy and initiatives, we speak to Dr Jong-Soo Choi, Chief Technical Officer, Office of Data & Digital Transformation at SMC. Dr Choi has led several large-scale IT projects at SMC, with a focus on emerging technology such as 5G, mobile, cloud, big data and AI. |
Q1: SMC aims to become the ‘model smart hospital of the world’. As a start, how do you define a smart hospital? What components or features set it apart?
Dr Jong-Soo Choi: Defining what constitutes a smart hospital is not easy. I believe the definition will vary depending on the perspective of each stakeholder involved in hospital operations.
For a networking company, it might be defined as having a technically robust structure that ensures uninterrupted service provision. For a pharmaceutical company, it might mean medications tailored to patients’ genetic characteristics to minimise side effects and complications. From a patient’s perspective, it could mean integrating data from their lifestyle to provide health management, disease prediction, and treatment services. A hospital that meets these diverse requirements from various stakeholders can be defined as a smart hospital from the hospital’s perspective.
(That being said), I believe the definition of a smart hospital is not static. It has and will continue to evolve alongside technological advancements.
Since its opening in 1994, SMC has been pursuing the concept of an advanced intelligent hospital, which is the precursor to the modern smart hospital, under the initiative known as “4-less”: Paper-less (through the HIS), Chart-less (EMR), Film-less (PACS) and Wait-less (Mobile applications).
Thirty years later, SMC is continuing this effort with the “Connect & Thru” concept.
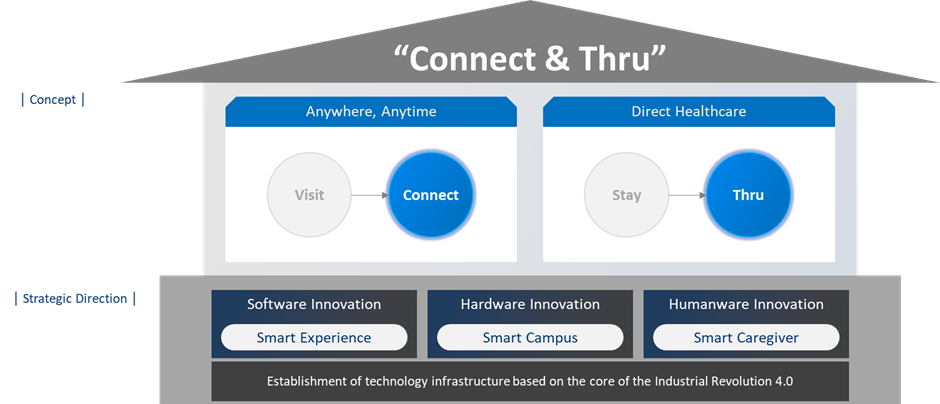
The fundamental concept is to provide services centred around the patient’s journey, to provide more convenience, speed, and efficiency for both patients and caregivers. For example, upon connecting to the hospital’s system, the patient doesn’t have to stand in queues or waste time waiting but can seamlessly navigate through the hospital.
Q2: What are the main challenges or risks in implementing smart hospital projects?
Dr Jong-Soo Choi: The most prominent challenges we face are technological maturity and sustainability.
In 2019, SMC piloted a system utilising 5G technology for surgical guidance. This system was designed to provide high-quality real-time video and audio of professors performing surgeries, for medical students to view in their lecture halls in real-time. However, it has not been able to expand further beyond the pilot.
The first challenge lies in the lack of robust technological maturity that can fully replace existing wired technologies. In addition, there is a need for alternative economic justifications for such significant investments to sustain continuous usage and promote further development.
But an example of how such challenges can be overcome would be our use of voice recognition technology to improve image reading efficiency.
In the past, interpreting medical images involved physicians viewing the images on PACS and verbally recording the reading results. A transcriber then listened to the recording and input the results into the system. The results go back again to the physician for review and confirmation. This process led to long turnaround time for results, slowed down subsequent stages of patient care, and made rectifying any inaccuracies inconvenient.
With voice recognition technology, radiologists in medical imaging can now directly input their reading results instead of relying on transcribers. In this case, both technological maturity and economic justification were achieved, leading to the stable integration and sustainability of the technology within the workflow.

Q3: Could you share some examples of smart hospital projects that have left significant impact on patient safety, experience or operational efficiency?
Dr Jong-Soo Choi: During the height of COVID-19, people were hesitant about in-person or physical contact. Using Robotic Process Automation, we automated the process of issuing medical record copies, which previously took up significant waiting time for patients.
Patients can obtain electronic copies and make online payments without visiting the hospital. For those who choose to collect physical copies from the counter, they can now do so within minutes instead of the previous hour-long wait.
A prominent example of enhancing patient safety is the AI solution Skinex (Skin Explainable AI). Skinex can analyse the severity of pressure ulcers and identify deep tissue damage based on photos of the affected area. It is also able to recommend appropriate dressing based on the condition. With an average of 200 patients suffering from pressure ulcers at any one time in our hospital (representing 10% of all inpatients), this solution helps relieve the workload of our pressure ulcer specialists.

Meanwhile, our smart hospital initiative is exemplified by our Data-based Operation and Communication Center (DOCC). DOCC integrates our medical resources, such as operating rooms and medical equipment, into a digital virtual hospital. It helps us deploy medical resources to the right place at the right time according to the current situation. For example, it predicts situations where patients may gather for blood tests and proactively assigns additional medical staff during those times to reduce congestion. It also reflects the availability of MRI or CT scan machines with the latest data on no-shows or appointments. This allows us to optimise our resources promptly and effectively.
Q4: What are the work priorities and projects for your team at SMC in 2024?
Dr Jong-Soo Choi: GenAI is undoubtedly the foremost focus. We are examining its applications across the patient journey, from appointment scheduling to outpatient care, examinations, surgeries, hospitalisation, and post-discharge management.
Determining which area to prioritise is still under consideration. At the end of last year, we took our first step by introducing Gen AI to our clinical data warehouse, which stores about 4.5 million patient data dating back from 1994. This would help us extract insights from specific data – for example, the effects of a particular drug on breast cancer patients.
Q5: How do you see smart hospitals evolving in the long-term?
Dr Jong-Soo Choi: Looking ahead to the next 20 or 30 years, we predict that changes will not only be driven by technological innovations, but also by content-based changes based on various big data such as lifelog data and genomic data. Furthermore, we anticipate a shift in roles and locations among hospitals, doctors, nurses, and patients.
I believe in the future, the role of the hospital will be changed as its many roles are not permanent. If we look back to the past, it was more common for doctors to visit patients’ homes. In 30 years or 50 years’ time, we may again see a change in situation.
The concepts of Home Hospital, Hospital at Home, and Care @ Home are not likely to become a reality in the near future. In South Korea, we will need changes in policies and more physicians (for this to happen), but I think our society and population needs this. Hospital at Home programmes have been found to offer several advantages over traditional inpatient care. Evidence from multiple randomised studies, both in the U.S. and internationally, supports these benefits, showing improved outcomes, decreased caregiver stress, and lower costs compared to traditional care.
In conclusion, in order to survive in the future of healthcare, it is essential to be well-prepared for even small technological changes and adapt to new environments. I consider this to be the fundamental concept of evolution.